Child Health Case Management
MCSP used the following strategies to ensure comprehensive case management of sick children in the countries where we worked:
Integrated Management of Newborn Babies and Childhood Illness
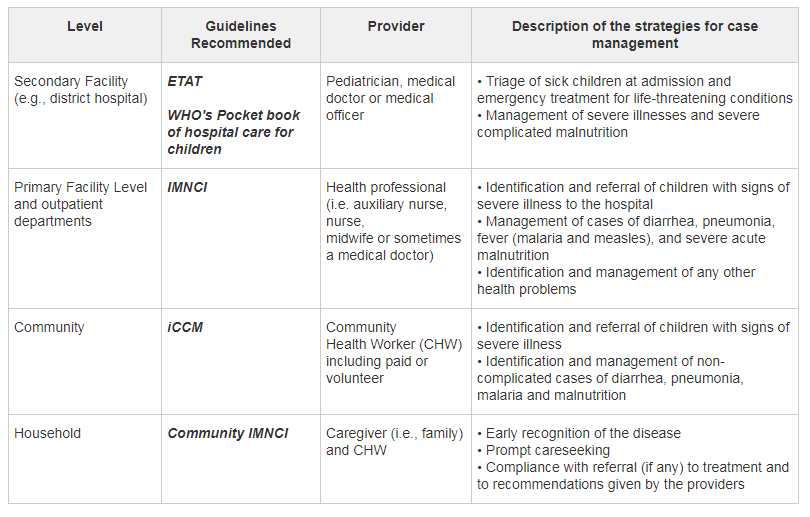
The cornerstone of case management for sick children is the Integrated Management of Newborn Babies and Childhood Illness (IMNCI). This strategy was developed in 1995 by the World Health Organization and UNICEF to promote health and provide preventive and curative services for children under-five in countries with greater than 40 deaths per 1,000 live births. At the heart of the IMNCI strategy is the treatment of the five common illnesses causing child deaths: pneumonia, malaria, diarrhea, malnutrition and measles. It is composed of three complementary components: improvement of health worker skills, strengthening of health systems, and improvement of household and community practices.
Integrated Community Case Management
In most countries with a high rate of under-five deaths, facility-based services alone do not provide adequate access to treatment — particularly within the crucial window 24 hours after onset of symptoms. For this reason, the community component of IMNCI was broadened to include a strategy to deliver lifesaving curative interventions for common childhood illnesses. This strategy is commonly known as Integrated Community Case Management (iCCM). The iCCM package varies from country to country, but it commonly includes management of diarrhea, pneumonia, malaria (where the disease is endemic), and screening for malnutrition. In the iCCM model, community health workers are selected and trained to identify children in need of immediate referral, and to assess and treat children with uncomplicated pneumonia, diarrhea and malaria.
Emergency Triage Assessment and Treatment
Emergency Triage Assessment and Treatment (ETAT) is the process of rapidly examining all sick children when they first arrive at a secondary facility in order to place them in one of the three following categories: children with emergency signs that require immediate emergency treatment, children with priority signs that should be given priority in the queue, and children with neither emergency signs nor priority signs that are non-urgent cases.