![]()
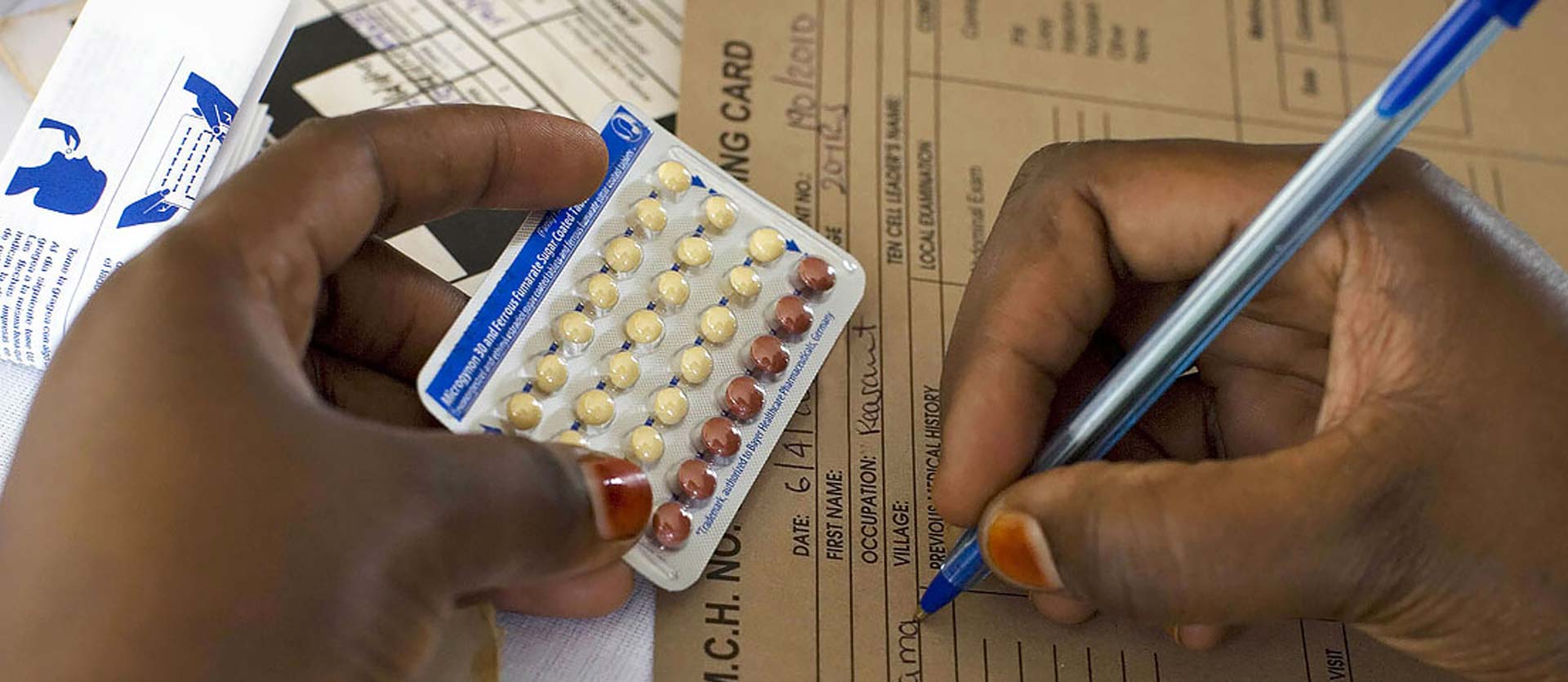
Reproductive Health
According to the World Health Organization’s world population estimates, 214 million women in developing countries currently wish to delay or prevent pregnancy, yet do not use contraceptives. The reasons for non-use are complex, involving social, cultural, and economic barriers, fears about side effects, and lack of access to a trusted provider. Greater access to family planning (FP) will be vital to achieving global goals in maternal health and child survival.
MCSP supported FP interventions in 20 countries. In facilities and countries where the Program worked, more than 750,000 clients accepted an FP method, including during a maternal, neonatal or child health visit. Our strategic approach for FP centered on accelerating achievements toward Family Planning 2020 and preventing child and maternal death goals by preventing unintended pregnancies, particularly those associated with poorer health outcomes. This included pregnancies occurring too soon after a birth, among high-parity women, and among older or adolescent mothers.
Pregnancies in youth and adolescents, for example, are linked with more adverse outcomes for both mothers and infants, including preterm birth, low birth weight, and perinatal and neonatal mortality. Moreover, rapid repeat pregnancies are more common in adolescents, making this population a key priority for MCSP.
Program key strategies included:
- Strengthening and scaling up postpartum FP (PPFP) and integration of FP along the maternal, newborn and child health (MNCH) continuum of care;
- Expanding method choice — including long-acting reversible and permanent methods — in FP and PPFP settings; and
- Reaching girls, their partners, and gatekeepers, whether they are mothers already or not, with appropriately targeted FP information and related care.
MCSP provided leadership to expand access to high-quality FP care and served as a global convening authority for documentation of best practices in FP/reproductive health programs. We advocated for and generated evidence around successful models that ensure every contact with a woman triggers a conversation about her reproductive intentions. At both health facility and community levels — in the context of care-seeking for herself or for her child — the aim was to link women to FP care whenever an unmet need was identified.
To address the global objective of closing innovation gaps, the Program worked on designing and field testing a number of innovations in relations to FP service delivery. These included:
- Testing new ways to capture PPFP counseling and uptake data, especially in contexts where the health information system does not capture key indicators and we cannot add supplemental registers;
- Learning around potential of hormonal intrauterine devices to contribute to improved access and use of contraception overall;
- Designing and field testing program models for engaging first-time and young parents grounded in rigorous formative research; and
- Designing and assessing models of integrated service delivery for FP and either immunizations services or nutrition services or both.